But it’s not new. Providers in college health probably understand, and experience, the health risks associated with travel more than in most health care settings. Our population travels a lot – across the state, across the country, and around the world. Then they all return to their campuses en masse several times each year, sometimes sharing recently acquired microbes with their fellow students, faculty, and the community.
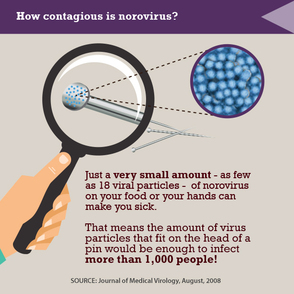
We should all be prepared to deal with the next big thing, including diseases exotic (chikungunya) or common (norovirus). If a student comes into your health center with a fever and reports recent travel to Africa, he or she is far more likely to have malaria than Ebola (and both have similar clinical presentations). But you’ll want to be able to respond effectively to either situation. There are some specific actions we can take now to prepare for what might show up this fall.
Here are a few ideas:
- Every health center should have emergency preparedness plans in place that include infectious diseases as a contingency. A single case of MERS-CoV – or even measles – would likely trigger a public health emergency response. Dust off old plans and update them accordingly.
- Providers should incorporate a simple travel history question to be asked of all patients with acute febrile illness (“have you traveled outside the United States in the last two weeks?”) and know what to do when the answer is “yes.” Generally, patients who develop specific signs and symptoms within 10 days of travel should be evaluated for the illnesses associated with the countries from which they traveled. Persons potentially exposed to someone with Ebola need to monitor their health for up to 21 days. Detailed guidelines for screening and management based on country and disease are posted on the U.S. Centers for Disease Control and Prevention (CDC) web site. If you use an electronic health record, you can add screening questions to note templates or as provider prompts.
- Establish appropriate infection control policies and enforce them. If available in your health center, utilize negative pressure isolation exam rooms for any patient with a cough illness. Make sure staff are trained in using personal protective equipment, properly fitted with respirators, and current on recommended immunizations.
- Identify someone in your health center to monitor CDC guidance and provide situation updates to staff. Stay abreast of travel recommendations. Sign up for electronic communications from the CDC’s Health Alert Network or the Center for Infectious Disease Research and Policy (CIDRAP).
- Build relationships and coalitions with your campus and community partners – student housing, study abroad programs, the international student office, student affairs, campus administration, public relations, plus local and state public health departments. Identify local experts and know who the point of contact is in your health department. Work with these partners to provide a consistent message to your students.
- Ensure your student population is highly immunized, with a special focus on international students. Recognize that many vaccine-preventable diseases – measles and pertussis in particular – are much more prevalent in other parts of the world. Develop the capacity to easily identify students at risk and consider sending targeted messages to them when needed. How quickly could you identify, notify, and potentially quarantine students susceptible to measles, should a case occur on your campus?
- If students are traveling abroad, both the U.S. State Department and the CDC provide country-specific advice regarding travel precautions. Keep your international study programs and students up to date with this information. It’s important to keep disease risk in perspective, though: motor vehicle accidents are the leading cause of death and injury for students in study abroad programs, not infectious diseases.
For More Information
Travel Health Resources








 RSS Feed
RSS Feed